The arterial baroreflex initiates with the beat-to-beat detection of variations in arterial blood pressure (BP) by the aortic and carotid baroreceptors. A rise in BP loads the stretch-activated baroreceptors, leading to parasympathetic nerve activation and sympathetic nerve inhibition. Reciprocally, a fall in BP unloads the baroreceptors, leading to parasympathetic nerve inhibition and sympathetic nerve activation. The consequent changes in heart rate (HR) and peripheral vascular conductance bring BP back to its set point pressure.
There are multiple ways to examine the arterial baroreflex function in humans:
Spontaneous baroreflex sensitivity
The cardiac component of the arterial baroreflex can be assessed by tracking spontaneous beat-to-beat fluctuations in systolic BP and the intervals between cardiac beats (i.e., R-R intervals). Sequences of three or more consecutive beats in which systolic BP and R-R intervals change in the same direction are identified as arterial baroreflex sequences. A linear regression is applied to each individual sequence and the slopes of the systolic BP and R-R interval relationships are averaged for a measure of spontaneous cardiac baroreflex sensitivity, with steeper slopes representing greater sensitivity of the baroreflex function.
Similarly, the sympathetic component of the arterial baroreflex can be assessed by tracking spontaneous beat-to-beat fluctuations in diastolic BP and muscle sympathetic nerve activity (MSNA). The values of MSNA (burst incidence or total activity) are averaged in bins according to their corresponding diastolic BP values. Then, a linear regression is applied between the diastolic BP and MSNA averages. A steeper slope represents greater baroreflex sensitivity.
Modified Oxford technique
This technique consists of the use of vasoactive drugs to drive BP beyond spontaneous fluctuations. A bolus injection of the vasodilator drug sodium nitroprusside, leading to a drop in BP and a reflex increase in HR and MSNA, is followed 60 s later by a bolus injection of the vasoconstrictor drug phenylephrine, thereby leading to a rise in BP and a reflex decrease in HR and MSNA. Then, beat-to-beat systolic and diastolic BP are plotted versus the corresponding HR and MSNA values, respectively. The slope of the linear portion of the relationship between BP versus HR or MSNA is used to estimate baroreflex sensitivity.
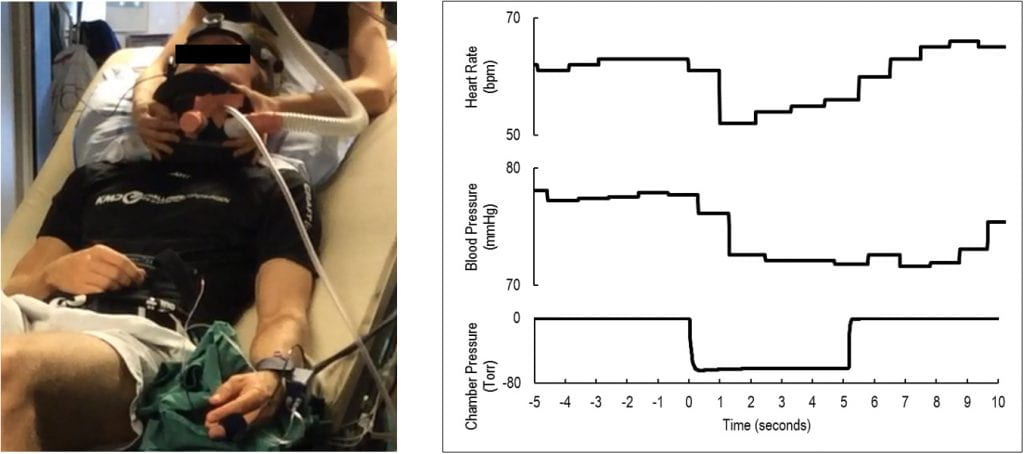
Variable pressure neck chamber
This non-invasive technique consists of a collar placed around the anterior 2/3 of the neck to isolate the carotid baroreceptor responses in humans. When pressure is delivered at the collar, the carotid sinuses are compressed and transmural pressure is decreased, leading to a simulated hypotensive stimulus and increases in HR, MSNA and BP. Reciprocally, when suction is delivered, the carotid sinuses are stretched and transmural pressure is increased, leading to a simulated hypertensive stimulus and decreases in HR, MSNA and BP.
Experimental Setup Example of Variable Pressure Neck Chamber:
Left: Example of experimental set-up using the variable pressure neck chamber. Right: Original tracing from one individual showing beat-to-beat heart rate and blood pressure in response to the application of neck suction at –60 Torr.